Please note: the guidance below is general in nature. Please discuss any specific concerns you may have with your clinician.
How effective is The Pill at stopping pregnancy?
All combined oral contraceptive pills in Australia have high efficacy, provided they are taken regularly. If taken 100% correctly, the contraceptive Pill is 99% effective at preventing pregnancy. However, when taken under we-are-only-human-and-not-capable-of-perfection (!) conditions, The Pill is about 91% effective over the course of a year. This means that, of 100 women taking The Pill for a year, 9 will become pregnant.
When taking The Pill, there are some things you can do to decrease the risk of unwanted pregnancy. These include:
– taking your pill at the same time each day: incorporating it into an existing daily routine may help, such as taking your Pill when you brush your teeth every morning
– considering shortening the number of days that you take the sugar pills, from 7 days to 4 days
– considering taking The Pill in a continuous or extended fashion (ie. taking 9 – 12 weeks’ of continuous hormonal tablets before taking a week of sugar pills). By running your pill packs together, you will reduce the risk of ovulation, should you accidentally miss a pill
Of course, please discuss the above approaches with your doctor. If you want an even more effective form of contraception, you may want to consider an intrauterine device, an implant, or even having your Fallopian tubes tied.
Non-contraceptive benefits of The Pill
In addition to providing reliable contraception, there are several additional (non-contraceptive) benefits that The Pill provides. Unfortunately, there is not a great deal of strong evidence to recommend one particular contraceptive pill brand over another, due to a relative lack of so-called ‘head to head’ studies, which directly compare specific pills to each other.
Lighter periods
Theoretically, all combined pills reduce both the duration and heaviness of periods. If you have previously been troubled by heavy menstrual bleeding, taking pill packets ‘back-to-back’ (ie. twelve or more weeks of continuous hormonal tablets, without any ‘sugar’ pills in between) can help. Doing so will lengthen the duration between periods, while also lightening your period when it does actually come.
Pills containing norethisterone (progestin) are generally considered to reduce bleeding more than pills that contain levonorgestrel (progestin). Hence, you could consider trialling a Pill that contains norethisterone, such as ‘Brevinor’ or ‘Norimin’ brand.
In the table above: the far left column displays the brand name; the second column lists the type and amount of oestrogen hormone in that pill; and the third column the progestin hormone. Pills that are subsidised by the Federal government’s pharmaceutical benefits scheme are in bold.
If you are taking a higher-dose pill, which contains 30 or 35 micrograms of ethinyloestradiol (oestrogen), it may be worth trying a pill with a lower oestrogen hormone dose – eg. only 20 micrograms of ethinyloestradiol. As mentioned above, oestrogen hormone acts to thicken the uterine lining. Logically, a pill that contains a lower oestrogen dose may not build up and thicken the uterine lining as much. Hence, your period may be lighter (or even non-existent) on a pill that contains a lower oestrogen dose.
The ‘Qlaira’ brand pill (which is a quadri-phasic pill containing oestradiol valerate as its oestrogen ingredient, and dienogest as its progestin), may reduce menstrual blood loss, due to its effect on the lining of the uterus. Compared to pills that contain ethinyloestradiol (oestrogen) and levonorgestrel (progestin), ‘Qlaira’ may be more effective at reducing both the number of days of bleeding, and the amount of blood loss. 30% of women who take ‘Qlaira’ experience no bleeding at all when taking the monthly ‘sugar’ pills.
If you have ongoing heavy menstrual bleeding despite taking an appropriate pill, your doctor may suggest having a pelvic ultrasound, to see if there are any other underlying causes to your heavy periods (such as fibroids, adenomyosis, or an endometrial polyp).
If you have ongoing heavy periods despite trying all of the above, you may want to talk with your GP about trying a progesterone-containing intrauterine device, such as a ‘Mirena’, which 90% of women find helps with heavy periods.
Less painful periods
Combined contraceptive pills have been shown to reduce period pain by 60% on average, and even up to 90% for women with severe period pain. As The Pill thins the lining of the uterus, the muscle of the uterus doesn’t need to contract as much, as there is less uterine lining to expel. Hence, trying The Pill may be an appropriate option if you are troubled by excessively painful periods.
In addition, you may want to consider taking your hormonal tablets ‘back to back’: up to 12 weeks of consecutive hormone tablets, before taking a week of ‘sugar’ pills. This means that you may have your period less often, so won’t have to suffer through a painful period every single month.
Lower risk of ovarian and endometrial (uterine) cancers
The use of The Pill is associated with lower rates of certain cancers, including endometrial (uterine), ovarian, and colorectal (bowel) cancer.
There is reasonable evidence that using the combined oral contraceptive pill decreases the risk of both ovarian and endometrial (uterine) cancer in future. Women who have used the combined pill at any stage have only two-thirds of the risk of ovarian or endometrial cancer in future, compared to women who have never used The Pill.
Women who are at particularly high risk of ovarian cancer (e.g. who carry a BRCA genetic mutation) are often encouraged to use The Pill, in order to decrease their risk of ovarian cancer somewhat.
One study conducted in the UK that undertook long-term follow-up of women who had and hadn’t ever taken The Pill estimated that Pill use resulted in the prevention of approximately:
– one third of ovarian cancers
– one third of endometrial (uterine) cancers
– and one fifth of bowel cancers
Fewer ovarian cysts
As the combined pill prevents ovulation, it also reduces the chances of developing some types of ovarian cysts: in particular, so-called ‘functional’, ‘simple’ or ‘physiological’ cysts (all names for the same thing). Such cysts can cause pain, and may even result in the ovary twisting (‘ovarian torsion’) and cutting off its own blood supply. Of note, The Pill has not been found to hasten the resolution of pre-existing ovarian cysts.
If you are prone to forming problematic ovarian cysts, you could consider trialling a contraceptive pill containing higher-dose (eg. 30 or 35 micrograms) of oestrogen.
Less acne and hirsutism (excess hair)
Most women who are troubled by acne or excess hair (the technical term is ‘hirsutism’) find that their skin improves when they take the combined pill. This is partly because the oestrogen in any combined pill increases production of a substance called ‘sex hormone binding globulin’, which mops up excess male hormones (testosterone) in the bloodstream, thereby improving acne.
In addition, the progestin ingredient in The Pill can also help to reduce both acne and excess hair. Some progestins are thought to be more or less ‘androgenic’ (ie. encouraging the development of male characteristics such as acne and excess hair) than others:
– norethisterone and levonorgestrel are considered more androgenic
– drosperione and cyproterone are considered ‘anti-androgenic’
Hence, Pills containing drosperinone or cyproterone may be the best option, if you are troubled by acne and/or hirsutism. Of note, this means that the progesterone-only pill that contains drosperinone (ie. ‘Slinda’) should also help to manage acne and excess hair.
While cyproterone-containing Pills are licensed for the management of severe acne or hirsutism, they do carry a slightly higher risk of venous thromboembolism (blood clots forming in your legs and / or lungs). As always, please discuss these finer points with your doctor: they may recommend using a cyproterone- or drosperinone- containing Pill for a few months until your acne improves, then changing to an alternative Pill (eg. containing norethisterone) that has a lower risk of blood clots, to take long-term.
Improved pre-menstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD)
Most women experience predictable emotional and mood changes, based on where they are in their menstrual cycle: for me, it’s having an extraordinarily low crying threshold in the few days prior to my period! A small proportion of women will experience more severe cyclic symptoms (known as ‘premenstrual syndrome’), and an even smaller percentage of women will experience severe dysphoric symptoms (premenstrual dysphoric disorder, or ‘PMDD’), which leads to depression and extreme emotional instability.
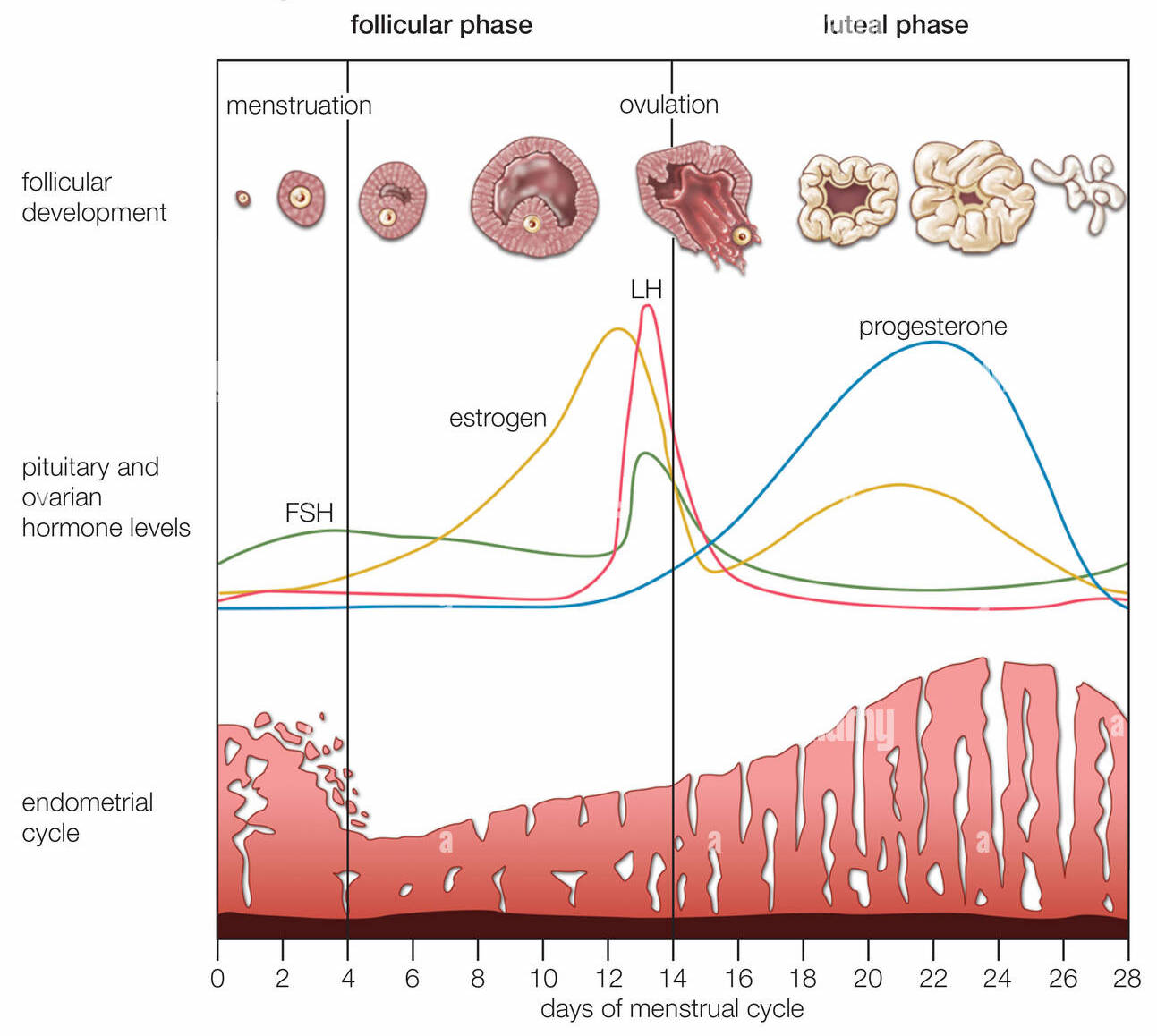
As you can see in the diagram below, ovulation occurs 14 days before your next period: for a stereotypical woman who has a 28-day cycle, then means she will ovulate on day 14. After ovulation, there is a dramatic increase in the level of both oestrogen and progesterone hormones (approximately day 21 on the graph below). If you didn’t get pregnant that month, these hormone levels then drop precipitously over the next few days (days 24 – 27): it is this rapid decrease in progesterone hormone that causes both PMS and PMDD symptoms, plus the period that occurs thereafter (on day 28).
Which begs the question: what impact does the contraceptive Pill have on these hormonal fluctuations, and women’s moods and emotions? Interestingly, one study found that over 70% of women on The Pill didn’t notice any change in their mood; the remaining 30% were split as to whether their mood worsened or improved.
Some researchers argue that ‘Yaz’ brand Pill may be more effective than other pills in treating severe premenstrual symptoms. Compared to placebo, it has been found to reduce impairment in productivity, social activities and relationships. This should be taken with a grain of salt, as there are very few ‘head to head’ studies that compare Pill brands directly.
Some women are exquisitely sensitive to progesterone, and may experience continuous PMS symptoms in response to the progesterone levels found in the contraceptive Pill (or ‘Mirena’ intrauterine implant). Of note, women with a history of depression are twice as likely than women who haven’t had depression previously to have a deterioration in their mood on The Pill. For such women, a non-hormonal form of contraception (such as the copper intrauterine device) may be more appropriate.
Some studies have shown that in women who are taking an antidepressant medication, contraceptive Pills that contain drosperinone (as their progestin ingredient) notice an improvement in their pre-menstrual symptoms. So trialling a pill such as ‘Yaz’ brand may be helpful.
Another option would be to try taking your Pill in a continuous or ‘back to back’ fashion, where you take 9 – 12 weeks of consecutive hormonal tablets, prior to taking your week of ‘sugar’ pills.
Endometriosis-related pain
There is limited evidence that, compared to other Pills, contraceptive pills that contain dienogest as their progestin ingredient (eg. ‘Valette’ or ‘Qlaira’) may better control pelvic and period pain in women with known endometriosis. This is because unlike some other progestin hormones, dienogest has no oestrogenic or so-called glucocorticoid activity.
Taking your Pill in a continuous or back-to-back fashion (eg. taking 9 – 12 weeks of hormone tablets, prior to taking a week of ‘sugar’ pills) can also help to reduce symptoms.
However, it’s important to note that when you eventually stop taking The Pill, any endometriotic implants (or ‘nodules’) are likely to become more active again, and symptoms return with a vengeance.
Taking the combined Pill after surgery for endometriosis can reduce the likelihood of any endometriotic cysts (or ‘endometriomas’) occurring again, and may also reduce the growth rate and size of endometriotic ovarian cysts that do occur again.
Conclusion
All combined contraceptive pills available in Australia are very effective at preventing unwanted pregnancy. Many are also purported to carry additional (non-contraceptive) benefits, such as: reduced risk of ovarian and bowel cancer; making periods lighter and less painful; helping to prevent some types of ovarian cysts; helping to acne and excess hair (hirsutism); and helping to manage premenstrual symptoms. There is limited evidence for some of these claims, so it’s important that you talk about your particular situation with your doctor, when working out which Pill is right for you.
The next blog post in this series will cover common side-effects from The Pill, and possible adverse events. Then the last blog in the series will cover frequently asked questions. So pour yourself another cup of tea, and read on!