Uterine fibroids are one of the most common gynaecological conditions, affecting up to two in three women by age 50. While many fibroids are harmless and cause no symptoms, others can lead to heavy bleeding, pelvic pressure, pain, or fertility problems.
For women who want relief from fibroid symptoms but wish to preserve their uterus — whether for future pregnancy or simply personal choice — laparoscopic myomectomy offers a safe, effective, and minimally invasive surgical option.
In this blog, we’ll explain what laparoscopic myomectomy involves, who it’s suitable for, what to expect before and after surgery, and how it compares with other treatment options.
What Is a Myomectomy?
A myomectomy is an operation to remove uterine fibroids (also known as myomas or leiomyomas) while preserving the uterus. Unlike a hysterectomy — which removes the uterus entirely — a myomectomy removes only the fibroids, leaving the uterus in place.
Fibroids are non-cancerous growths that develop from the muscle of the uterus. They can vary in size, number, and location:
- Subserosal fibroids grow on the outer wall of the uterus
- Intramural fibroids are within the uterine wall itself
- Submucosal fibroids project into the uterine cavity
Fibroids are common during the reproductive years and often shrink after menopause. However, when they cause troublesome symptoms, surgical removal may be recommended.
What Is a Laparoscopic Myomectomy?
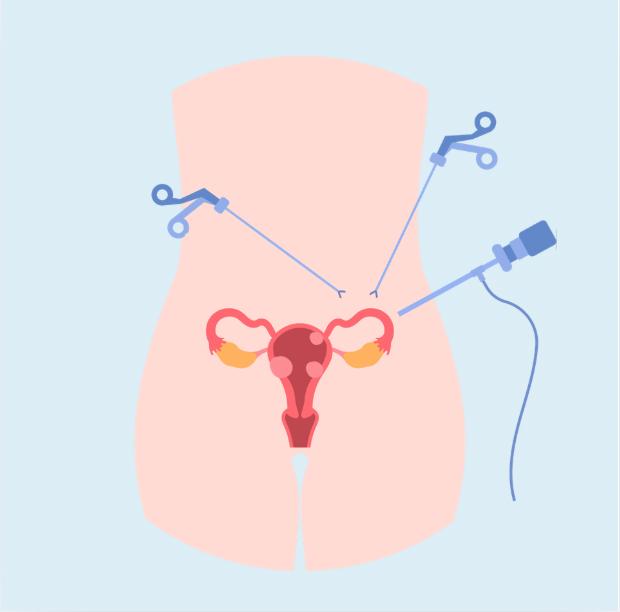
A laparoscopic myomectomy is a minimally-invasive way to remove fibroids using a camera and fine surgical instruments inserted through a few small cuts in the abdomen — usually three or four incisions, each less than one centimetre long.
The surgeon fills the abdomen with gas (carbon dioxide) to gently lift the abdominal wall and provide space to work. A laparoscope (a thin telescope with a camera) gives a magnified view of the uterus. Using long, delicate instruments, the surgeon carefully removes the fibroids and then repairs the uterus with dissolvable stitches.
The fibroids are then removed through the small incisions, often using a process called morcellation, where they are broken into smaller pieces inside a contained device for safe extraction.
Laparoscopic myomectomy is performed under general anaesthetic, usually taking between one and three hours depending on the number and size of fibroids.
Who Might Benefit from Laparoscopic Myomectomy?
Laparoscopic myomectomy may be suitable if you:
- Have symptomatic fibroids, such as heavy bleeding, pelvic pain, bloating, or pressure
- Wish to retain your uterus for fertility or personal reasons
- Have fibroids up to around 10 cm, or a small number of fibroids (suitability depends on their size and position)
- Are otherwise healthy and suitable for keyhole surgery
It may not be the best option if you have very large or numerous fibroids, severe pelvic adhesions from prior surgery, or if fibroids are deeply embedded in areas difficult to reach laparoscopically.
Your Maven Centre gynaecologist will arrange imaging — usually an ultrasound or MRI scan — to map the fibroids and determine which surgical approach is safest and most effective for you.
Benefits of Laparoscopic Surgery
Compared with open (abdominal) surgery, laparoscopic myomectomy offers several advantages:
- Smaller incisions and minimal scarring
- Faster recovery — most women return to normal activities within 2–4 weeks
- Less pain and blood loss
- Shorter hospital stay — typically one night, occasionally day surgery
- Lower risk of infection or adhesions (internal scar tissue)
The uterus is preserved, allowing for future pregnancy if desired.
How to Prepare for Surgery
Before surgery, your doctor may recommend:
- Blood tests to check for anaemia (since heavy bleeding is common with fibroids) and general health
- Pelvic imaging (ultrasound and/or MRI) to confirm the number, size, and location of fibroids
- Pre-operative medications, such as a short course of hormone therapy (GnRH analogues), to shrink fibroids and reduce blood loss during surgery
- A discussion about recovery, fertility goals, and potential risks
You’ll also be asked to fast before your operation and to arrange for someone to drive you home afterwards.
What to Expect During and After Surgery
During Surgery
Under general anaesthetic, the laparoscope and instruments are inserted through small incisions — one near the belly button and others lower in the abdomen. Fibroids are located and carefully dissected out of the uterine wall. The uterus is then reconstructed with dissolvable sutures to maintain its strength and integrity.
The procedure typically lasts between one and three hours. The lengthy of surgery depends on the size and location of the fibroid which impacts complexity.
Morcellation
Once the fibroid has been removed from the uterus, and the uterus reconstructed, a bag is placed inside the abdomen, into which the fibroids are placed.
The fibroids can then be removed in one of two ways:
- Manual morcellation: the fibroids are cut into smaller pieces manually using a knife, so that these can be removed through a smaller incision
- Power morcellation: the fibroids are cut into smaller pieces using a power tool inside the bag
After Surgery
Most women wake up with mild abdominal discomfort, bloating, and shoulder tip pain from the gas used during the procedure. These symptoms usually settle within a few days.
You’ll stay in hospital for a short period — often just overnight — while pain control and recovery are monitored.
Recovery at Home
- Pain and energy: Expect mild to moderate pain for a few days; this is usually managed with oral pain relief.
- Activity: Gentle walking is encouraged, but avoid heavy lifting, strenuous exercise, and sexual intercourse for 2–4 weeks.
- Bleeding: Light vaginal bleeding or discharge for up to 2 weeks is normal.
- Work: Most women can return to work after 2–3 weeks, depending on occupation.
A post-operative check (typically 4–6 weeks after surgery) ensures the uterus is healing well and that your symptoms are improving.
You can read our detailed post-operative guide on our website.
Potential Risks and Complications
While laparoscopic myomectomy is generally very safe, as with all surgery there are potential risks, including:
- Bleeding, occasionally requiring transfusion
- Infection
- Injury to nearby organs such as the bladder, bowel, or ureters
- Scar tissue (adhesions) forming inside the pelvis
- Recurrence of fibroids — new fibroids may grow later in life
- Conversion to open surgery — if there is unexpected bleeding or technical difficulty
Your surgeon will discuss these risks with you and explain how they are minimised.
Fertility and Pregnancy After Myomectomy
One of the key advantages of myomectomy is that it preserves fertility. Many women who undergo laparoscopic myomectomy go on to have healthy pregnancies.
Depending on the depth of fibroids removed and how the uterus was repaired, your doctor may recommend:
- Waiting 3–6 months before attempting pregnancy, to allow full healing of the uterine wall
- A planned caesarean birth for future deliveries, to reduce the risk of uterine rupture during labour (a rare but serious complication)
Your gynaecologist will provide personalised advice based on your surgery and fertility plans.
Alternatives to Laparoscopic Myomectomy
For some women, other treatment options may be more suitable. These include:
- Hysteroscopic myomectomy – for fibroids inside the uterine cavity
- Open (abdominal) myomectomy – for very large or numerous fibroids
- Uterine artery embolisation (UAE) – a radiological procedure that blocks blood flow to fibroids (not recommended if you wish to preserve fertility)
- Medical therapy – such as hormonal treatments, the Mirena® IUD, or tranexamic acid to manage heavy bleeding, GnRH agonists or Ryeqo
Each approach has its benefits and limitations, and your gynaecologist will help tailor the best plan for your individual needs and fertility goals.
Final Word
Fibroids are common — but they don’t have to define your comfort, confidence, or fertility. Laparoscopic myomectomy combines precision, effectiveness, and faster recovery in a modern, uterus-preserving approach.
If you’re struggling with fibroid symptoms or exploring fertility-preserving options, speak with your GP or one of our gynaecologists at Maven Centre. We’ll assess your fibroids, discuss all available options, and guide you through a treatment plan that supports your health, your future, and your peace of mind.